Racist Cop Handcuffs Black Paramedic Mid-Emergency – Jury Awards $18.6M
.
.
Racist Cop Handcuffs a Black Paramedic Mid-Emergency
The Night “Working a Code” Was Ignored—and a Jury Awarded $18.6 Million
The words should have ended everything.
“Working a code.”
In emergency medicine, those words don’t invite discussion. They don’t open debate. They don’t wait for permission. A code means cardiac arrest—no heartbeat, no circulation, no margin for delay. It means hands on a chest, compressions steady and deep, oxygen pushed where a heart can’t. It means seconds deciding futures.
On that evening, those words were spoken clearly, calmly, and repeatedly.
And they were ignored.
Seconds That Matter
The crash sat at the edge of dusk, cones flaring orange against blood-speckled asphalt. A sedan rested at an awkward angle, glass glittering under floodlights. Sirens faded into background noise—the steady chaos of a scene already under control by first responders.
Kneeling beside the patient was a paramedic, gloved hands locked into rhythm, shoulders over chest, compressions counted without counting because the cadence lived in muscle memory now. The cardiac monitor screamed its truth—flatline. Oxygen hissed. Sweat beaded at his temples. He did not look up. He could not.
A life depended on his hands continuing.
Then boots cut between the cones.
The body camera snapped on mid-jog. The timestamp blinked alive. The flashlight was already on, though the scene was lit bright enough to read license plates. The beam skimmed debris—chrome, glass—then climbed, not to the patient, but to the man kneeling.
“Hey.”
The greeting wasn’t coordination. It was confrontation.
The paramedic didn’t stop compressions. He lifted his left palm a fraction—acknowledgment without interruption—and spoke the words that should have closed the moment.
“Working a code.”
Bias Before Assessment
The officer’s posture said decision before information. Shoulders high. Chin tucked. Dominance forward. He planted himself where sterile space had been carved for resuscitation, boots wide at the patient’s feet.
The flashlight lingered—too long—on the paramedic’s back, then slid across equipment anyone on an emergency scene recognizes instantly: trauma shears on the belt, radio mic on the shoulder, turnout pants streaked with road grime. The gear was visible.
It was ignored.
The beam snapped to tattoos on the paramedic’s forearm. Paused there. The priority skewed catastrophically.
“Stand up.”ư

The command overlapped the monitor’s flatline alarm—the sound that means compressions are the only thing moving blood. The order was not just unreasonable. It was lethal.
The paramedic shook his head once. Small. Minimal. The smallest refusal that allowed compressions to continue.
“Working a code.”
When Explanation Becomes “Defiance”
Crowd murmurs swelled as bystanders realized what they were watching. A horn blared somewhere behind the cones. Oxygen hiss threaded the audio.
The officer’s hand moved to his cuffs. Metal clicked against the belt.
This was the second escalation.
The flashlight dipped to the paramedic’s wrists—the wrists attached to the hands keeping someone alive. The beam ignored the patient’s face entirely. A seed of regret flickered, unspoken and overridden.
The paramedic turned just enough to show the patch stitched to his turnout coat.
“Paramedic.”
One word. Clear. Identifying.
He did not stop compressions.
The officer stiffened. Authority challenged hardened into resolve.
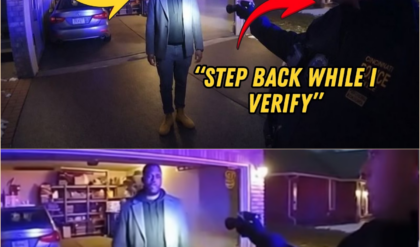
“Step away.”
The hands left the chest.
For the first time since arrival, compressions stopped.
The monitor screamed.
Handcuffs bit shut around latex gloves.
Metal scraped against the protective layer that kept the rescuer sterile. The gloves—evidence of medical function—were now evidence of restraint. The cuffs tightened. Not released. Tightened.
“He’s EMS!” a bystander shouted.
Ignored.
The officer adjusted the cuffs again, committing to the error.
“You’re detained.”
The Moment Care Ended
The paramedic stood, cuffed, breathing controlled by discipline rather than panic. His eyes flicked once to the patient. A micro-nod of apology passed unseen.
The chest lay still.
What had been minutes—precious, narrowing minutes—slipped away without hands to replace a heart’s function. The monitor’s alarm dominated the soundscape, an electronic scream marking the loss of time that cannot be refunded.
Backup sirens dopplered in. Chaos spiked. The officer’s flashlight wandered without purpose now, the control narrative fraying.
Then came the choice that turned catastrophe into cruelty: the cuffs were tightened again after recognition—after the patch, after the words, after the bystanders’ confirmation.
The patient did not survive.
What the Camera Proved
The investigation was the most exhaustive the department had ever conducted. Frame by frame. Word by word. Opportunity by opportunity.
The findings stacked, irrefutable:
Active CPR was visible and audible.
Chest compressions were underway when the officer intervened.
Explicit identification was given.
“Working a code.” “Paramedic.” Both clear, technical, unmistakable.
Equipment was present.
Trauma shears, radio mic, gloves—ignored.
Commands ordered cessation of life-saving care.
“Stand up.” “Step away.”
Handcuffs were applied to gloved hands mid-CPR.
Care stopped because restraint made it impossible to continue.
Bystander confirmation was ignored.
“He’s EMS!”
Cuffs were tightened after recognition.
Error became deliberate conduct.
Medical experts testified with brutal clarity: interruptions in CPR slash survival odds—7 to 10 percent per minute. The minutes without compressions materially reduced the patient’s chance to live.
The chain of causation—from handcuffs to death—was documented.
Criminal Accountability
This did not end with internal discipline.
Criminal charges followed—rare, and warranted by consequence:
Interference with emergency medical services (felony)
False imprisonment
Assault
Criminally negligent homicide (reduced from manslaughter)
Convictions came. Prison time followed. Certification was permanently revoked. The officer’s name entered every database that tracks misconduct. A law-enforcement career ended with a criminal record.
The Civil Trial
The civil case ran separately, brought by the paramedic and the patient’s estate.
The claims were precise and devastating:
Fourth Amendment: unlawful seizure while performing medical duties
Fourteenth Amendment: race-based enforcement
Assault and battery: restraints applied and tightened after recognition
Intentional infliction of emotional distress: forced to watch a patient die
Wrongful death: interruption of care causing loss of survival chance
The jury did not blink.
$18,600,000.
The breakdown told the story the verdict could not soften:
$2.4M — Paramedic compensatory damages
$4.2M — Paramedic punitive damages
$7.5M — Estate compensatory damages
$4.5M — Estate punitive damages
Among the largest awards for a single-officer encounter—because the harm extended beyond civil rights into the realm of life and death.
Aftermath and Legacy
The paramedic returned to duty. He carries the memory of the patient he could not save—the seconds that slipped away when his hands were taken.
The footage became mandatory viewing nationwide. Training academies pause the video at three moments:
“Working a code.”
Trainees learn: cardiac arrest in progress. Do not interfere.
“Stand up.”
Trainees learn: stopping compressions kills. Orders must yield to medicine.
The cuffs tightening.
Trainees learn: commitment to error is catastrophe compounding.
The lesson is simple and unforgiving:
Emergency scenes have medical professionals.
CPR cannot be interrupted.
The person kneeling over a body might be saving that body’s life.
Two words should have stopped everything.
“Working a code.”
They were heard—and dismissed.
The cost was measured not only in dollars, but in a human life that might have been saved if bias had yielded to recognition, and authority had yielded to care.